The kidneys are vital organs in the body, responsible for filtering blood, removing waste, and maintaining a balance of fluids and electrolytes. They are part of the urinary system, which also includes the ureters, bladder, and urethra. In addition to producing urine, the kidneys play an essential role in regulating blood pressure, red blood cell production, and electrolyte balance.
This article will explore the anatomy of the kidneys and their functions, focusing on how they filter blood and produce urine.
Overview of Kidney Function
The primary function of the kidneys is to filter blood and remove waste products, excess fluids, and electrolytes from the body in the form of urine. They maintain homeostasis by regulating fluid balance, electrolytes, and blood pressure. The kidneys also produce hormones that support other vital functions, such as the regulation of red blood cell production and calcium metabolism.
Key Functions of the Kidneys:
- Filtration: Removes waste products and excess substances from the blood.
- Reabsorption: Returns necessary nutrients, water, and electrolytes back to the bloodstream.
- Secretion: Releases certain ions and compounds into the urine.
- Excretion: Eliminates waste in the form of urine.
- Regulation: Maintains fluid balance, electrolyte levels, and blood pressure.
- Hormone Production: Produces hormones like erythropoietin (stimulates red blood cell production) and renin (regulates blood pressure).
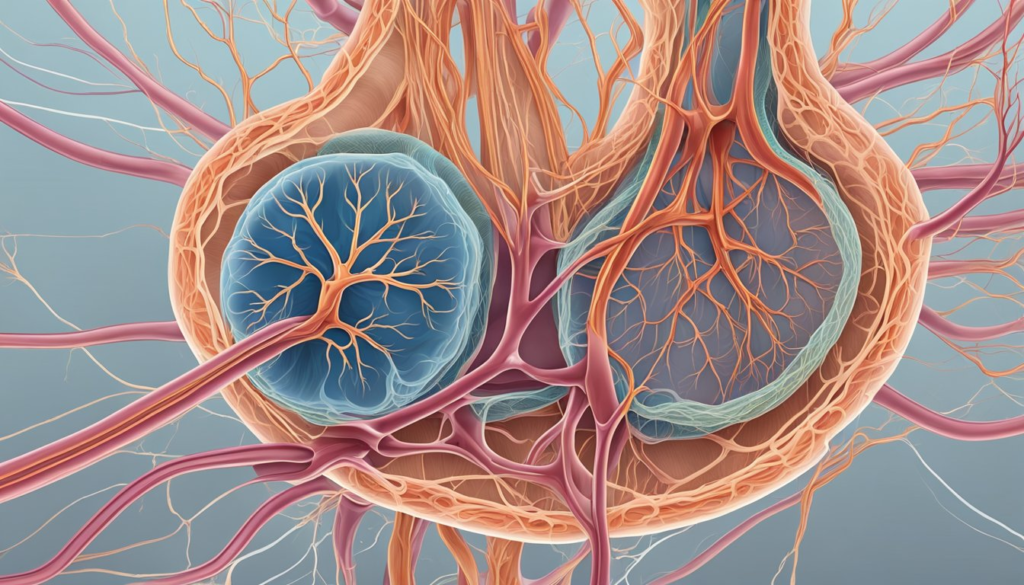
Anatomy of the Kidneys
Each kidney is a bean-shaped organ located in the back of the abdominal cavity on either side of the spine. They are about the size of a fist and are protected by layers of fat and the ribcage. The kidneys are composed of several key structures that work together to filter blood and produce urine.
External Structure
- Renal Capsule: A thin, tough outer layer that protects the kidney.
- Renal Hilum: The indented region on the medial side of each kidney where the renal artery, renal vein, and ureter connect to the kidney.
Internal Structure
The internal structure of the kidney can be divided into three main regions: the renal cortex, renal medulla, and renal pelvis. Each region plays a specific role in filtering blood and producing urine.
1. Renal Cortex
The outermost layer of the kidney, the renal cortex contains nephrons—the functional units responsible for filtering blood. The cortex also houses blood vessels that transport blood into and out of the nephrons.
2. Renal Medulla
Located beneath the cortex, the renal medulla is composed of cone-shaped structures called renal pyramids. These pyramids contain the tubules and collecting ducts that carry urine from the nephrons to the renal pelvis.
3. Renal Pelvis
The renal pelvis is a funnel-shaped structure located at the center of the kidney. It collects urine from the collecting ducts and channels it into the ureter, which then carries the urine to the bladder.
The Nephron: Functional Unit of the Kidney
The nephron is the functional unit of the kidney, responsible for filtering blood and forming urine. Each kidney contains approximately one million nephrons, each of which consists of several components that work together to filter blood and balance the body’s fluid and electrolyte levels.
Key Components of the Nephron:
- Glomerulus: A network of tiny blood vessels (capillaries) where filtration of blood begins. The glomerulus filters water, ions, glucose, and waste products from the blood.
- Bowman’s Capsule: A cup-shaped structure that surrounds the glomerulus and collects the filtrate (filtered fluid).
- Proximal Convoluted Tubule (PCT): The first segment of the nephron tubule where most of the reabsorption of water, ions, and nutrients occurs.
- Loop of Henle: A long, U-shaped portion of the nephron that plays a key role in concentrating urine by reabsorbing water and salts.
- Distal Convoluted Tubule (DCT): The final segment of the nephron tubule, responsible for further adjusting the composition of urine, including reabsorbing sodium and secreting ions.
- Collecting Duct: The last structure in the nephron, which collects urine from multiple nephrons and transports it to the renal pelvis for excretion.
Filtration Process in the Nephron
The process of urine formation occurs in three main stages: filtration, reabsorption, and secretion.
1. Filtration
Filtration begins in the glomerulus, where blood pressure forces water, ions, glucose, amino acids, and waste products through the glomerular capillaries into Bowman’s capsule. This fluid is called filtrate, and it contains both waste products and essential substances that need to be reabsorbed.
2. Reabsorption
As the filtrate moves through the nephron, essential substances like water, glucose, and ions (sodium, potassium) are reabsorbed into the bloodstream through the walls of the proximal convoluted tubule and Loop of Henle. The reabsorption process ensures that the body retains necessary nutrients and maintains fluid and electrolyte balance.
3. Secretion
In the distal convoluted tubule, certain ions and waste products are secreted from the bloodstream into the nephron to be eliminated. This process helps maintain the body’s acid-base balance and ensures that excess waste is excreted.
Once the filtrate has passed through the nephron and reached the collecting duct, it is now considered urine. The urine is transported to the renal pelvis and then through the ureter to the bladder for storage and eventual elimination.
Blood Supply to the Kidneys
The kidneys receive a rich blood supply through the renal arteries, which branch off from the abdominal aorta. Each renal artery enters the kidney at the hilum and further divides into smaller arteries and arterioles, which deliver blood to the nephrons for filtration.
Key Blood Vessels in the Kidneys:
- Renal Artery: Supplies oxygenated blood to the kidneys.
- Afferent Arterioles: Deliver blood to the glomerulus for filtration.
- Efferent Arterioles: Carry blood away from the glomerulus after filtration.
- Renal Vein: Drains deoxygenated blood from the kidneys and returns it to the inferior vena cava.
Efficient blood flow to and from the kidneys is essential for the filtration process and maintaining the body’s internal balance.
Urine Formation and Excretion
The kidneys play a crucial role in the formation of urine, which is the primary method of removing waste products and excess substances from the body.
Steps in Urine Formation:
- Filtration in the Glomerulus: Blood is filtered in the glomerulus, and the resulting filtrate enters the nephron.
- Reabsorption in the Tubules: Essential nutrients and water are reabsorbed into the bloodstream in the proximal tubule and Loop of Henle.
- Secretion in the Distal Tubule: Excess ions and waste products are secreted into the nephron to be removed.
- Excretion via the Collecting Duct: The final urine passes through the collecting ducts into the renal pelvis and is transported to the bladder through the ureters.
Once urine reaches the bladder, it is stored until it is excreted from the body through the urethra during urination.
Hormonal Regulation of Kidney Function
The kidneys are involved in regulating several hormones that help control blood pressure, red blood cell production, and calcium balance.
Key Hormones:
- Renin: Produced by the kidneys in response to low blood pressure, renin triggers a series of reactions that lead to the production of angiotensin II, a hormone that constricts blood vessels and raises blood pressure.
- Erythropoietin (EPO): The kidneys produce erythropoietin to stimulate red blood cell production in the bone marrow when oxygen levels in the blood are low.
- Calcitriol: The kidneys convert vitamin D into its active form, calcitriol, which helps regulate calcium absorption in the intestines and maintains healthy bones.
Conclusion
The kidneys are essential organs that filter blood, remove waste, regulate fluid and electrolyte balance, and produce urine. Through the work of nephrons, the kidneys ensure that the body maintains homeostasis and stays free of harmful waste products. Understanding kidney function is key to appreciating their vital role in overall health and wellness.
Frequently Asked Questions (FAQ)
What is the primary function of the kidneys?
The primary function of the kidneys is to filter blood, remove waste products, and maintain fluid, electrolyte, and acid-base balance in the body. The kidneys also produce urine to eliminate waste.
What is a nephron, and why is it important?
A nephron is the functional unit of the kidney responsible for filtering blood and producing urine. Each nephron performs the essential processes of filtration, reabsorption, and secretion, which are critical for maintaining the body’s internal environment.
How do the kidneys help regulate blood pressure?
The kidneys regulate blood pressure by producing the hormone renin, which activates a pathway that leads to the constriction of blood vessels, raising blood pressure. They also adjust the balance of fluids and electrolytes, which affects blood pressure levels.
What happens if the kidneys stop functioning properly?
If the kidneys stop functioning properly, waste products and excess fluids build up in the body, leading to conditions like uremia, hypertension, and fluid overload. Chronic kidney disease can result in kidney failure, requiring dialysis or a kidney transplant.
How much blood do the kidneys filter each day?
The kidneys filter approximately 150-180 liters of blood per day, removing waste products and excess substances while reabsorbing essential nutrients and water.
What role do the kidneys play in red blood cell production?
The kidneys produce the hormone erythropoietin (EPO), which stimulates the production of red blood cells in the bone marrow in response to low oxygen levels in the blood.